Where Can Nurse Practitioners Work Without Physician Supervision?
Since the inception of the first nurse practitioner (NP) education program in 1965, men and women in the profession have experienced great success and heated opposition. Physician organizations have openly opposed the use of nurse practitioners as primary care providers, claiming that educational gaps render NPs unsafe and unqualified to care for patients independently.
Even though the decades-old debate continues, research has proven time and again that nurse practitioners are indispensable primary care providers with the ability to treat a wide variety of conditions. Moreover, the Kaiser Family Foundation (KFF) indicates that 58 million Americans live in areas in which the supply of primary care physicians doesn’t meet federal standards with the appropriate ratio of providers to patients. The gap is widening as legislation expands access to medical care, and the Association of American Medical Colleges (AAMC) predicts the physician shortage could reach up to 139,000 physicians by 2033. Nurse practitioners are gaining independence and establishing autonomy as they provide medical care without the oversight or management of a physician.
What Is Scope of Practice for Nurse Practitioners?
The American Nurses Association (ANA) defines scope of practice as the “services that a qualified health professional is deemed competent to perform, and permitted to undertake — in keeping with the terms of their professional license.”
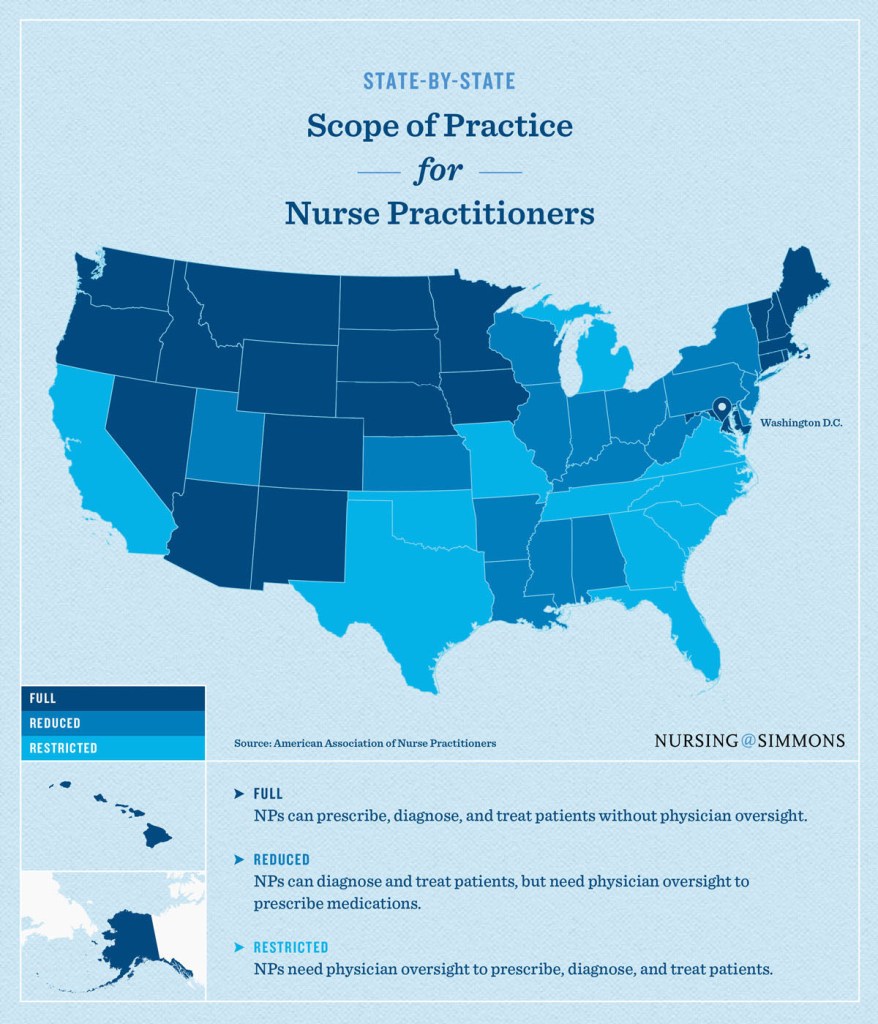
The three types of practice regulations for NPs are:
FULL: NPs can prescribe, diagnose, and treat patients without physician oversight. Nurse practitioners who operate in full-practice states are also allowed to establish and operate their own independent practices in the same way physicians do.
REDUCED: NPs can diagnose and treat patients but need physician oversight to prescribe medications.
RESTRICTED: NPs need physician oversight to prescribe, diagnose, and treat patients.
Nurse Practitioner Scope of Practice by State
Scope of practice guidelines for advanced nursing professions vary by state. Currently, 22 states and the District of Columbia have approved “full practice” status for nurse practitioners, a provision that allows them to assess, diagnose, interpret diagnostic tests, and prescribe medications independently.
Kaiser Health News reports that Alaska, New Hampshire, Oregon, and Washington were the first states to offer expanded scope of practice NPs in the 1980s; more rural states, mainly those with physician shortages, followed in the 1990s.
Note: The following scope of practice designations are accurate as of April 28, 2021.
Full-Practice Authority States
- Alaska
- Arizona
- Colorado
- Connecticut
- District of Columbia
- Hawaii
- Idaho
- Iowa
- Maine
- Maryland
- Massachusetts
- Minnesota
- Montana
- Nebraska
- Nevada
- New Hampshire
- New Mexico
- North Dakota
- Oregon
- Rhode Island
- South Dakota
- Vermont
- Washington
- Wyoming
Reduced Authority States
- Alabama
- Arkansas
- Delaware
- Illinois
- Indiana
- Kansas
- Kentucky
- Louisiana
- Mississippi
- New Jersey
- New York
- Ohio
- Pennsylvania
- Utah
- West Virginia
- Wisconsin
Restricted Authority States
- California
- Florida
- Georgia
- Michigan
- Missouri
- North Carolina
- Oklahoma
- South Carolina
- Tennessee
- Texas
- Virginia
Expanding Nurse Practitioner Practice Status
In 2010, full practice status became the recommended model by the Institute of Medicine and the National Council for State Boards of Nursing. Not all states, however, are on board with the measure; 27 continue to mandate reduced or restricted practice regulations for nurse practitioners. While the guidelines for reduced and restricted practice regulations are slightly different depending on location, both require NPs to have either a signed collaboration agreement with a physician or direct oversight from a physician. Not all states require the physician to be physically present or even in the same building with the NP during patient care, but they should be available by phone or email.
Despite aggressive opposition from the medical community, new and changing legal policies indicate that lawmakers are looking closely at the NP’s role in expanding coverage to underserved areas and easing the burden on the dwindling number of primary care physicians who remain — calling the NP role “necessary for long-term health care.”
More than 20 states expanded NPs’ practice ability through legislation or regulation in 2013, according to the 26th Annual Legislative Update from The Nurse Practitioner. Several states have also approved new legislation for NPs that empowers them to sign death certificates and formal health records.
With the approval of SB 61 in 2017, South Dakota became the latest state to pass legislation allowing nurse practitioners to practice independently.
Additionally, states aren’t the only entities moving to dismantle practice barriers: In 2016, the U.S. Department of Veteran Affairs (VA) issued a proposal that would “permit full practice authority of all VA advanced practice registered nurses (APRNs) when they are acting within the scope of their VA employment.”
Communication and Collaboration in the Future
Health care leaders from nursing and medicine fields agree that there should be more conversations addressing the independence of NPs. Both sides concur that the NP role is vital to the health and delivery of medical care in this nation, but neither can agree on the best way to achieve the goal. As both sides hold strongly to their convictions, there is sure to be more debate — and potentially more autonomy — for nurse practitioners.
Additional Career Resources:
Citation for this content: Nursing@Simmons, the online FNP program from the Simmons School of Nursing


